Sepsis, a common and potentially deadly complication to an infection, is the leading cause of death in U.S. hospitals, accounting for 35% of in-hospital deaths.
But as many as 87% of sepsis cases originate outside the hospital, according to the Sepsis Alliance. And when the condition advances to septic shock, it can kill people within 12 hours. That’s why it’s important to recognize its signs and symptoms early.
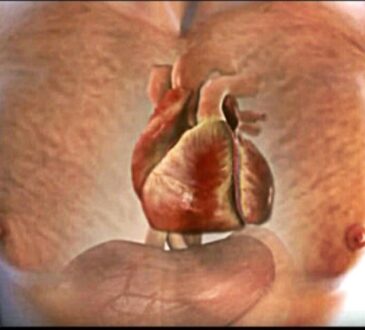
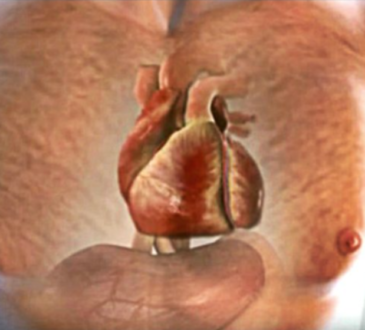
Sepsis is an extreme bodily response to an infection. This overreaction triggers overwhelming inflammation and blood clots, which can block the delivery of oxygen and nutrients throughout the body. It can lead to organ and tissue damage.
Older adults, infants and people with weakened immune systems and medical conditions like diabetes, obesity, cancer and kidney disease are among those most at risk.
Any type of infection can turn septic, but it is more common with infections of the lungs, urinary system, digestive system, bloodstream, wounds and catheter sites.
The signs and symptoms of sepsis
Signs and symptoms include confusion or disorientation, shortness of breath, rapid heart beat, fever, extreme pain and clammy skin. The Sepsis Alliance uses the acronym TIME to help people remember them:
T – higher or lower than normal temperature
I – infection
M – mental decline (the person is confused and sleepy)
E – extremely ill (the person is in severe pain or discomfort, struggling to breathe)
Without proper treatment, sepsis can spread throughout the body unchecked, causing the lungs, kidneys, liver and other organs to malfunction.
In severe cases, the infection may spread to the brain. When a patient goes into septic shock – the most severe form – blood pressure plummets, leading to organ failure or death.
Many people who survive sepsis are left with complications such as post-traumatic stress disorder, organ dysfunction, and chronic pain and fatigue. Sepsis also causes many people to have amputations.
Sepsis death rates generally declined in the United States from 2000 to 2019, according to the U.S. Centers for Disease Control and Prevention.
In 2019, there were 201,092 deaths involving sepsis, with the greatest number of deaths occurring people 65 and older. But the risk increased with age: People age 85 and older were 5 times more likely to die of sepsis than adults ages 65-74.
In 2020, sepsis caused 2,277 deaths in Pennsylvania and 2,061 deaths in New Jersey.
Preventing and treating sepsis
The earlier the treatment for sepsis, the better the outcomes. The chance of sepsis progressing to septic shock and causing death increases 4-9% for every hour the treatment is delayed.
Treatment typically involves intravenous fluids and antibiotics. More serious cases may require a breathing tube, kidney dialysis or surgery.
There have not been any new drugs developed in the last 30 years that have improved patient outcomes, despite research efforts. Sepsis patients have different immune system responses, and their bodies react differently to varying treatments.
The best way to prevent sepsis is to practice good hygiene, proper wound care and management of chronic conditions, and to stay current on all immunizations, according to the CDC.
What causes sepsis?
Scientists still don’t completely understand the underlying mechanisms that lead to organ failure and death. It is still not clear why the body sometimes has a severe inflammatory response to an infection, but other times does not.
One study suggests that blood glucose levels may play a role. When these levels are not properly regulated, the body’s resilience against infection is lowered, the researchers found.
Other studies have found that the severity of sepsis – and how far it progresses – partly depends on where the infection is and the type of infection. One study found that patients with bacteremia, peritonitis and pneumonia are mostly likely to go into septic shock.